In her mid 20s, Chandell was diagnosed with a lung disease that causes inflammation and scarring (fibrosis) of the lungs. Prior to the diagnosis, Chandell attended college and was successful in her career as a Production Lead for Schweitzer Engineering…
Sandee Rudy’s enthusiasm and zest for life is evident as she describes her and husband Scott’s shared passion for cycling. Last year alone, Sandee logged an impressive 3,000 miles on her bike.

Chris Magera grew up with a mobility disability. As a child, she had multiple surgeries, but as an adult, she has worked hard to maintain an independent personal and professional lifestyle. Chris lives with her husband, Dale, on a farm with many animals. She enjoys horseback riding, camping, rafting, and entertaining her five grandchildren. Professionally, Chris works full-time in a leadership position for a very busy regional healthcare system and enjoys her work.
While walking into work this winter, Chris slipped and fell on the ice, sustaining a distal femur fracture. The injury required a very complex surgical repair, and post-operatively Chris experienced great difficulty with mobility. She knew that to return home safely, she had to be stronger. Inpatient rehabilitation offered Chris that opportunity.
When asked why she chose Rehabilitation Hospital of the Northwest (RHN), Chris said, “I live in Idaho and have worked with RHN for many years. I know the quality of their work and have had many friends and some family utilize RHN’s services over the years. To me, RHN was the ONLY choice.”
When reflecting on her experience, Chris found her expectations weren’t just met, but exceeded. “I was so well cared for, from nursing, PCTs, therapies, the kitchen team, and everyone else. The overall environment at RHN promotes healing and positivity.”
Chris also spoke of many staff that impacted her stay at RHN, from several nurses who went above and beyond to assist with her pain, especially at night, to the biggest connection she formed with Jenelle, a physical therapist. “She challenged me every day to try just a little more and helped me with the confidence I needed to get up and move.” Chris stated that she also would like to recognize Alyssa, one of RHN’s occupational therapists. “Alyssa has such a no-nonsense way about her and really thinks outside the box on how to accomplish things. With her help, I had no doubts I could manage at home and in the kitchen.” Finally, Chris wanted to recognize Tim, RHN’s van driver. “We had some adventures for sure. He was so attentive and there was a lot of snow to deal with, but he just took it in stride and got me where I needed to go. He truly watched out for me. He was such a pleasure to be around,” she said.
Success for Chris is getting outside again, walking greater distances without pain, riding her horse again, and returning to work fully. Since leaving RHN, Chris has achieved her goals one by one. She has gone from wheelchair level to a walker and now walking with a cane, and she has put away all of the durable medical equipment in her house. “I am driving. I am socializing. I am going in to work in-person a day per week.”
Chris loves to travel and looks forward to some of the “bucket list” trips she has planned with her husband. She also has a new kayak just waiting for her to take it to the river.
“We are very fortunate in north Idaho to have RHN,” Chris stated. “The services they provide to our community are top-notch. The staff at RHN truly care about the patient. I can’t recommend them high enough.”

With her kids grown and moved out of the house, Diane Eberly was in her fifties and looking for a new hobby. She found a horse rescue in her hometown in Pennsylvania and began volunteering. Diane loved working with the horses and started taking lessons in western pleasure riding. Shortly after, she became the owner of her first horse, General.
Diane and her husband, Ed, also loved to travel. They liked to vacation in Idaho, Montana, and Wyoming and fell in love with the area. They moved to northern Idaho when she was 69 to be closer to family and to enjoy an active outdoor lifestyle. Shortly after arriving, her second horse, Scooter, a seventeen-year-old Belgium Draft, made the trip to northern Idaho.
One beautiful summer day, Diane and her husband went out for a ride. Ed was capturing pictures of her and Scooter when the unthinkable happened. She fell from her horse and suffered a major traumatic spinal cord injury. Ed immediately called 9-1-1 and the ambulance took her to Kootenai Hospital. She spent nearly a week there undergoing surgeries and starting her long road to recovery.
Luckily, Diane was wearing a helmet that protected her brain when she fell. However, her spine suffered multiple injuries that required extensive surgery. This included laminectomy, discectomy, plating, fusing, and caging for several of her cervical vertebras, as well as spinal cord decompression. Several days later, Diane also had to have surgery on her wrist.
Diane’s surgeon was optimistic but knew that she had an intense recovery ahead of her. Post-surgery, Diane was unable to utilize her fine motor movements in both hands and experienced numbness. She was on a robust pain regimen and required a Hoyer lift for transfers out of bed. She required a cervical collar for additional protection and to restrict movement. Because of her condition, Diane needed assistance with her activities of daily living.
When Diane reflects on her initial days at Kootenai, she didn’t remember much. She couldn’t even recall the accident and was just thankful to be alive. Five days after the accident, she was discharged from Kootenai Hospital and admitted to Rehabilitation Hospital of the Northwest.
Diane knew she was going to have to work hard to see improvements. “I had to progress. What else was I supposed to do except work with what I have left? You have to keep moving forward,” she explained.

Over the next four weeks, Diane had to re-learn how to do things like getting in and out of bed, walking, and eating and writing with her non-dominant hand. She made great progress and was thankful for the full support from the RHN staff. “The team was very attentive to all of my needs,” she said. “I want to thank everybody that helped me.” When she was first admitted, she was dependent for all care. At discharge, she ranged from moderate assist to supervision for most cares.
A friend of Diane’s flew in from Pennsylvania to help her the first two weeks she was home. She had a total lifestyle change and needed assistance with her daily routine. Her family built a wheelchair ramp for easy entrance to the house. They also worked on a sleeping and bathing setup that was suitable for the cervical collar she had to wear 24/7. North Idaho Home Health came in to continue managing her medical and rehabilitation needs. Even though she was not used to relying on others for this much help, she was thankful for the support from her family, friends, and the home health company.
Diane’s hard work and determination paid off. She is now walking with a cane, can shower by herself, and can write with her non-dominant hand. She attends outpatient therapy two days a week and participates in aquatic therapy. In the spring, she is hoping to get back on her horse so she can utilize equine-assisted therapy, or hippotherapy.
“If my story can help motivate anyone facing this type of life-changing situation, I am glad to share it,” Diane shared. “I would tell them, don’t give up! You might think you can’t do it, but you can! Your body is an amazing thing!”

After an extended hospitalization, Calvin Dustybull chose Rehabilitation Hospital of the Northwest to help him regain his function and indpendence.
After undergoing heart surgery, Calvin Dustybull had a complicated recovery. Calvin has a complex medical history, including coronary artery disease, mitral stenosis, chronic atrial fibrillation, and diabetes with advanced chronic kidney disease. The 62-year-old faced a long and complicated recovery before he could safely return home to his two sons in Browning, MT.
Twenty days after a quadruple coronary artery bypass grafting, Calvin still needed a high level of medical care. He required a ventilator, dialysis, and an NG tube for feeding. He also suffered from encephalopathy (altered mental state) and thrombocytopenia (low blood platelet count). For self-care activities, Calvin required the assistance of others.
Calvin needed a hospital that specialized in managing medically-complex patients like himself. His care team at Benefits Hospital in Great Falls, Montana referred him to Northern Idaho Advanced Care Hospital (NIACH).
At NIACH, Calvin began to make progress in his recovery. The pulmonary intensivist team and clinicians weaned him off the ventilator. Soon, he was decannulated and breathing room air. Over the course of five weeks, Calvin received dialysis three times per week. With nutritional support and therapies, his strength improved. Except for a slight memory deficit, Calvin’s encephalopathy resolved, as well.
Calvin recalls the staff at NIACH encouraging him to work hard and keep fighting each day. “At the beginning, I couldn’t speak or remember my name,” Calvin said of his admission to NIACH. “But with the help of therapies and encouragement from the staff, I remained focused on my goals and my memory started to improve.”
With a strong foundation to build on, Calvin was ready for the next stage of his recovery. However, his needs remained great. Calvin’s care plan required continued hemodialysis, therapy for strengthening, wound and stoma care, anticoagulation management, diabetic management, and continued nutritional support. This led Calvin to Rehabilitation Hospital of the Northwest (RHN). RHN shares a campus with NIACH in Post Falls. There, Calvin would receive the medical care he needed while receiving more intensive therapy. For three hours each day, Calvin received physical, occupational, and speech therapy at RHN.
Throughout his stay at RHN, Calvin made great strides in his recovery. He increased his independence with transfers and activities of daily living. His mobility improved to ambulating 120 feet with a four-wheel walker. Speech therapy helped address his mild cognitive defects. Calvin also made progress with his diabetes. He no longer required insulin, with his hemoglobin A1C down to 5.8.
Calvin attributes his great outcomes to goal setting and the team approach at both NIACH and RHN. He expressed appreciation for the education he received, as well. The staff taught Calvin about his medical conditions, medications, exercises, and assistive devices. They also shared ways to increase his safety, strength, and function at home. This education carried over to his loved ones, as well. On Calvin’s discharge day, his two sons and a friend participated in caregiver training. Staff informed them of necessary follow-up appointments they had set for Calvin, too.
Calvin and his loved ones were excited for his return home. They planned a cookout with his grandkids and friends to celebrate his success. Calvin continues to gain additional strength each day, utilizing the education he received at NIACH and RHN.
It was a journey that would forever change their lives.
At 4:00 a.m, Barb Hollace took one look at her husband and said, “You’re not OK.” Her husband, 74-year-old Bill Hollace, had been coughing for a couple of days and was not looking good that morning. Barb called an ambulance. Bill was taken to Valley Hospital in Spokane Valley, WA where he was diagnosed with pneumonia. That night, the hospital staff informed Bill that they thought he was having a heart attack, despite the fact that he wasn’t feeling any symptoms. Three days later, while still at Valley Hospital, he was diagnosed with Influenza A. The following morning he had a stroke.
Bill was immediately transferred to Deaconess Medical Center where he underwent surgery. Deaconess and Valley Hospital are both a part of the MultiCare Hospital system. All strokes within the MultiCare system are transferred to Deaconess, which is the only Spokane hospital to have earned the Joint Commission Stroke Certification.
Bill spent the next 50 days at Deaconess in the intensive care unit as he recovered from his multiple health issues. About two weeks into his stay, he was placed on a ventilator due to respiratory failure. The Hollaces received what they described as great care from a dedicated staff.
During Bill’s stay in ICU, there were a lot of conversations about next steps, such as discharging to a skilled nursing facility who could manage a ventilator. But after ongoing conversations between Barb and several ICU nurses, it was suggested that Bill needed to transfer to North Idaho Advanced Care Hospital (NIACH) in Post Falls, Idaho. Although this would mean moving Bill out of their home state, in Barb’s mind, her greater concern was Bill’s care.
Dr. Coulston, Medical Director, Intensive Care Unit at Deaconess also recommended NIACH because of its reputation and high standards. Barb trusted Dr. Coulston with Bill’s life and highly valued his opinion. Ultimately, after looking at the NIACH website and reviewing testimonials, Barb chose to continue Bill’s journey at NIACH. Barb said, “We had to finish his journey well. Nothing less than top-rate care was acceptable. We needed to give Bill the best chance at life.”
Great care is what they got at NIACH, according to Barb. “The very first day that we were at NIACH, we were getting work done,” said Barb. “The trach was downsized; we were working on mobility.”
Barb also commented that “the respiratory therapists at NIACH have the system down. They know when to push. Not too far, but still stretching the envelope. NIACH provided an amazing opportunity for him to get weaned off the ventilator, and step by step getting closer and closer to his recovery.” The Hollaces also found that the medical providers went above and beyond by working consistently through the Easter weekend to secure a pacemaker placement for Bill. The pacemaker was a huge step forward in Bill’s recovery process.
Una Alderman, CEO of NIACH, would wave at Barb when she saw her arrive. “Una made it personal. Everyone there did, from housekeepers to the front desk, we had the best. We received so much encouragement and affirmation along the path.” Bill added, “They made me feel like I could beat this. They were the support right there to encourage and push.”
Barb recalled hearing someone say, “Miracles happen here, all the time.” Bill was named the “Miracle Man” at Deaconess because of his amazing recovery. Barb knew they were in the right place at NIACH.
From the very beginning of this journey, Barb’s belief was that Bill would walk again. At first, Bill wasn’t able to participate as much as he would have liked to with physical therapy, due to the magnitude of his medical issues at the time. The Hollaces, though, were hopeful that Bill would soon be able to participate with therapy in such a way that he could transfer to the Rehabilitation Hospital of the Northwest (RHN). RHN is the sister facility to NIACH and sits on the same campus.
To accomplish this, the Hollaces, when medically ready, chose to continue their “Road to Rehab” at Life Care Center in Post Falls (a skilled nursing facility) in hopes of increasing his strength and endurance for admission to RHN. Bill hit a bump in the road during his two weeks at Life Care with a reoccurrence of his pneumonia. “We took a little detour and got to come back to NIACH a second time,” Barb said, “which on one hand was a bummer, but on the other hand, how cool is that! Bill was able to start eating and advancing his diet during that second time, and he was able to do more physical therapy. Then, we got to go to RHN to “polish the diamond” is what I liked to call it.”
According to Barb, coming to RHN was a different experience. “Three hours a day of therapy…kind of like boot camp, huh, Mr. Bill?” she chuckled to her husband. “Coming to RHN was a blessing; they encouraged family members to be there. We learned so much from family involvement and training.” Family members are encouraged to stay there, which Bill found as a great opportunity “to see if we were still compatible.”
Bill remembers the daily, jovial jousting between himself and the RHN therapists. He would say, “Let’s challenge me.” And they would. Bill wanted to be challenged as he didn’t want to get bored. Bill talked about how the therapists at RHN didn’t make him feel like he was part of the masses or only a number. They were there for him and his individualized care. Bill said, “They made fun out of it and that helped the stress back away.”
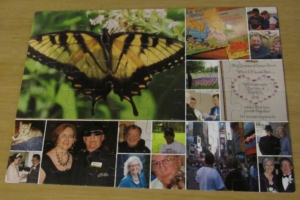
Barb made this puzzle, filled with memories of their past, to help Bill with his memory during recovery. The butterfly represents the transformation that has occurred and hope for the future.
There were tough moments, too. Barb called them the “breakthrough parts.” There was a “blow up” when he was working with the speech therapist on math, using coins. Bill said, “I need to have a way to measure my progress.” They started recording his progress on a chart on the bathroom door. It was very beneficial for Bill to see his progress. It helped him to understand why he was there and doing what he was doing. Bill felt as though he was a part of the team instead of only doing things that he was told to do.
In preparation for Bill’s discharge to home, Erik, a physical therapist at RHN, went to Bill and Barb’s home to do a home evaluation to see what obstacles Bill might encounter when he returned home with his wife. They realized that going up eight stairs to their second-story apartment was very challenging. It had the potential to be a dangerous situation for both Bill and Barb, as she assisted him up and down the stairs. Erik and Bill returned to the gym to practice on the stairs. Bill was able to discharge to his home with his wife. At first, going from a whole team of caregivers to the two of them at home was a big adjustment.
About a week after discharge, the Hollaces moved to a ground floor apartment that eliminated this high-risk for fall situation. The Hollaces were able to utilize home health physical, occupational, and speech therapy, as well, as he adjusted to being home in his own environment. Barb commented that her training time at RHN with Bill was an invaluable resource for their transition to life at home.
Barb recalled that their first stop after leaving RHN was Wendy’s for a hamburger. For months, when Bill was receiving his nutrition via a stomach feeding tube, he often dreamed of having a hamburger. It may have been the best hamburger Bill has ever eaten.
Currently, Bill is using a front-wheeled walker and a four-wheeled walker, when needed. Working with a home health physical therapist, Bill is increasing his stamina and expanding his territory to longer distance walks outside. Some days, the therapists work with Bill to walk in their home without walker assistance for distances up to 200 feet.

The Hollaces renewed their wedding vows in 2012. Their love and support of each other played an important part in Bill’s recovery.
The Hollaces attend church every Sunday. Wednesdays and Saturdays are their adventure days. At first, those days consisted of only driving around, maybe they got something to eat or drink and sat in the parking lot. Bill and Barb tried to do things that wouldn’t overstimulate him as they gradually reintroduced Bill to the world outside the hospital, where he had spent five and a half months. They set goals about when and where they would go and accomplished them one by one.
Bill acknowledged how very scary this process was. He said, “I wouldn’t wish this on my worst enemy.” Bill served in the United States Marine Corps, and as he described it, that even after his service and everything else, even being fired at by the best, “They did a lot of damage, but they couldn’t do the damage that this little bug did to me.”
Bill expressed his thankfulness, as well, wishing to be able to thank everyone who helped him along the way. He hopes that others will have the same opportunities that he did to help them get better. Barb reaffirmed, “What a great opportunity! There were great people at both facilities that really made this journey just so amazing for us. We felt so supported. What a blessing! We wouldn’t be where we are today, except for all their help.”
Today, the Hollaces look forward to enjoying the spring and summer with more walks outside and time in the park. “Life is precious. We are grateful every day for Bill’s life and his ongoing recovery, “ Barb said with a smile. “The best is yet to come.”

Jamie Smith leaves RHN after completing therapy for learning to balance and walk with his new prosthetic.
Jamie Smith grew up in sunny Southern California. Standing at a height of 6’5” he enjoyed playing high school football and basketball. As Jamie grew into adulthood, he made a living working as a truck driver in the oil fields of West Texas and Colorado. After 25 years, Jamie relocated to Rathdrum, Idaho to be closer to his mother and sister. During that time he developed a love for some lifetime hobbies including golf, fishing, and motorcycles.
During this time, Jaimie spent a lot of time climbing up and down from his rig. This earned Jamie bilateral total knee replacements. “It took me 58 years to wear out those joints,” Jaimie said with a chuckle. Unfortunately for Jamie, he required a revision of that first knee replacement and developed a serious infection. That revision would become the second of a frustrating eight surgeries. This resulted in two years of severe pain which left Jamie unable to walk, let alone enjoy the hobbies he loved so much.
Jamie consulted with local orthopedic surgeon Dr. Joseph Bowen, and ultimately chose to have an above-the-knee amputation. Now that Jamie was close to his family and had a good support network intact, he felt he could make the decision to amputate with confidence. “One day I am going to be back in my daily game,” Jamie said to himself. “Even though it wasn’t going to happen with my natural limb, I need to get back with the common day, communication, not institutionalized, sitting at home by myself, with no chance to use my humor. I don’t want to say ‘I wish I would have…’.”
After the amputation, Jamie chose to transfer to the Rehabilitation Hospital of the Northwest (RHN) in Post Falls, Idaho. He was at RHN for ten days. Jamie worked with the physical and occupational therapists on wheelchair level training and how to safely balance with a front wheeled walker. His goal was to return home and be functional at wheelchair level until he could get his custom prosthetic limb.
Upon admission to RHN, Jamie indicated he was very scared and anxious about falling. But he soon found he was in good hands. “The staff here were very helpful,” Jaime said. “I didn’t have anything to worry about as they made sure I was safe.”
According to Jamie, the staff made sure he was comfortable, too. To accommodate Jaime’s height, the staff got him a larger bed. He said, “I slept like a baby from that day forward.” Jamie also stated that he enjoys being able to eat in the Bistro with the other patients. “The food is good, very good, dependable as there is always a choice. Eating and visiting with the other patients is helpful.” Before Jamie discharged home, RHN case managers/social workers coordinated continued care at home via Panhandle Home Health. They would help Jamie adjust to being home and functioning from a wheelchair and continuing his therapy.
Jamie chose to return to the Rehabilitation Hospital of the Northwest once his custom prosthetic limb was ready. He would need to learn how to balance and walk with his prosthetic.
“I’ve been to a few hospitals with this. This has been the BEST hospital I have been to,” Jamie said of RHN. “I have observed other patients in physical therapy and everyone treats them so well. [The therapists] know what they are doing, very professional. They explain WHY they are doing what they are doing, so that I understand.” He also said, “you can tell the therapists, the nurses, the whole staff, they love their jobs. They have been so encouraging and they gave me so much respect. They show all of the patients respect. Even the doctors. Dr. Duba comes in every day to see me. He checks in on me mentally, physically, and addresses it all then.”
“I am so glad that I came in for inpatient rehab. I’m motivated, but not as much as they motivate me here.” He also said, “goal setting is a must. If you don’t hold yourself accountable, it’s easy to fall into a laziness and it’s difficult to get back into working hard, getting back into your surroundings. They make it fun. I don’t think that I would have been as motivated at home, by myself, to do what I have done here. They push me to my goals, and my goal…is to walk out of here!”
Jamie is looking forward to getting back on the golf course. He just wants to swing the club and give his friend a good game. He also says that he is looking forward to getting out on his friend’s brand new fishing boat to do some fishing.
“I have a lot to look forward to,” Jamie added. “It’s gonna be okay.”
Rehabilitation Hospital of the Northwest has been named in the Top 10 percent of inpatient rehabilitation facilities in the United States for the 4th year in a row. The hospital’s care was cited as being as being patient-centered, effective, efficient and timely.
“We strive to deliver this higher level of care as our standard,” says Jennie Pipoly, Chief Operating Officer, Rehabilitation Hospital of the Northwest. “We have graciously been recognized as a top performing facility for many years now, but we never take it for granted.”
“Our staff is exceptionally passionate about helping patients reach their full potential through the care we provide,” says Maureen Fakinos, Interim CEO and Senior Vice-President of Operations. “We work daily to ensure patients are reaching their highest levels of ability and independence.”
Rehabilitation Hospital of the Northwest was ranked in the Top 10 percent from among 870 inpatient rehabilitation facilities nationwide by the Uniform Data System for Medical Rehabilitation (UDSMR), a non-profit corporation that was developed with support from the U.S. Department of Education, National Institute on Disability and Rehabilitation Research. The UDSMR maintains the world’s largest database of rehabilitation outcomes.
“If you take into account that a national study has previously shown that inpatient rehabilitation facilities provide better long-term results for patients, being ranked at the top of that group validates the quality of care we provide,” says Dr. Steve Foster, Associate Medical Director for Rehabilitation Hospital of the Northwest, referencing a study commissioned by the ARA Research Institute that showed patients treated in inpatient facilities experienced improved quality of life as compared to skilled nursing facilities.
“To provide the highest level of rehabilitative care available to our own community is truly rewarding,” says Dr. David Duba, a physical medicine and rehabilitation physician at the hospital. “This means our family, friends, and colleagues don’t need to leave the area to receive this level of care.”
Through the UDSMR, Rehabilitation Hospital of the Northwest also will collaborate with peers throughout the nation to share information and establish best practices for patients. “This helps elevate rehabilitative care for everyone across the United States,” Duba says.
Rehabilitation Hospital of the Northwest provides specialized rehabilitative services to patients who are recovering from or living with disabilities caused by injuries, illnesses, or chronic medical conditions. This includes, but is not limited to, strokes, brain injuries, spinal cord injuries, orthopedic injuries, cerebral palsy, ALS (Lou Gehrig’s Disease), multiple sclerosis, and Parkinson’s disease.
During the long and harsh winter, which required what felt like endless hours of snow removal and clean-up, Coeur d’Alene resident Greg Nelson had a stroke.
His wife Jane Nelson noticed something was not right after he spent a January afternoon clearing snow out of the driveway. She recognized the signs of a stroke and they immediately sought help, since quick action and treatment offer the best chances for survival after a stroke and recovery from stroke-related disabilities.
The effects of his stroke initially left Greg unable to walk, speak properly and more.
Jane Nelson knew that they needed to find the best therapy care around for his recovery.
Greg Nelson went to the Rehabilitation Hospital of the Northwest located in Post Falls, Idaho.
“The level of care at Rehabilitation Hospital of the Northwest matched the level of care that we needed,” Jane said. “Greg is a type-A, over-achieving and I knew he needed the intensity of therapy offered here for the fastest recovery possible.”
At the rehab hospital, Greg was assigned a care team that worked collaboratively together to get him home as quickly as possible, ensuring he could get back to the highest level of independence attainable. The care team for a stroke patient like Greg usually includes a case worker, doctor, nurses, physical therapist, occupational therapist and a speech therapist.
Greg was impressed all around with his entire team.
“They always made sure I did everything I was supposed to do. Even when I didn’t think it was something I was ready for yet, they knew exactly how to push me to just the right level. I am thrilled about my recovery,” he said.
The rehab hospital provides patients with 24-hour rehabilitation nursing care and daily physician management.
Greg Nelson had a private patient room and access to well-equipped therapy areas. The therapy areas include a 2,360-square foot therapy gym with private treatment rooms, a heated aquatic therapy pool with an electric lift, and a therapeutic courtyard to allow practice on different terrains such as ramps, stairs, gravel, dirt, curb, curb cut-outs, and wood decking.
“My favorite therapy exercises were the arm bike and the stairs,” he said.
He worked with his team in these state-of-the-art therapy areas every day during his stay. His occupational therapist Melissa Ching focused on self-care goals that would help get him home and gain independence in activities.
“Greg is a hard worker. He was always dedicated to his therapy during his stay,” she said.
He also worked with Candice Frank, a physical therapist. With Greg’s stroke affecting his right side they focused on rebuilding and retraining it with forced use. She helped him stay safe and work at a safe pace for recovery.
“One of our goals is to help patients avoid falling, which can lead to other injuries. We also remind our patients and work with their family to help them know what to watch for when they return home,” she said.
Greg Nelson also worked with Cheri Rose-Kociela, a speech therapist. Her work covers more than just speech: memory, thinking process, actual speech production, language and swallowing.
“I didn’t realize that learning how to swallow properly again would be something that was part of therapy,” he said.
Most of the speech therapy is based on the patient being as functional as possible.
“Sometimes my work also includes teaching patients how to use tools like a smartphone as a memory device, setting alarms and using the calendar function,” Rose-Kociela said.
Most people don’t realize it, but stroke is the leading cause of serious, long-term disability in the United States. In fact, approximately 795,000 people suffer a stroke each year according to the American Heart and Stroke Association.
About 610,000 of these are first attacks, and the rest are recurrent attacks. While strokes can happen at any age, research shows that nearly three-quarters of all strokes occur in people over the age of 65. The risk of having a stroke more than doubles each decade after the age of 55.
The American Stroke and Heart Association released new guidelines strongly recommending that stroke patients be treated at inpatient rehabilitation facilities. The guidelines highlight the effective and important aspects of rehabilitation from an inpatient rehabilitation facility, including:
• Patients participate in at least 3 hours of rehabilitation a day from physical therapists, occupational therapists, and speech therapists
• Nurses are continuously available
• Doctors typically visit daily
The guidelines advocate for patients to go to inpatient rehabilitation hospitals because there is considerable evidence that patients benefit from the team approach in facilities that understand the importance of rehabilitation during the early period after a stroke.
Greg Nelson’s stay at Rehabilitation Hospital of the Northwest was only about two weeks. He made great strides in gaining back his ability to walk, speak and perform self-care activities independently.
In fact, he walked out of the rehab hospital using a walker; and now several months later he only needs a cane when out and about.
“But I can walk around the house without one.” His wife Jane is happy to see him smiling again and getting back to his usual self. Greg notes, “I’m even back to walking the dog now.”
—
(photo) Greg and Jane Nelson visit Rehabilitation Hospital of the Northwest. Greg was a patient there following a stroke in January.
Alan Golub was starting to feel depressed about his situation.
A stroke had robbed him of movement on the left side of his body and impacted his speech.
He didn’t know if he would be able to walk or continue with his artwork. The Hayden resident was determined to recover, but the seeds of doubt were growing.
Then his doctor got hold of Golub’s mandolin and asked him to play. Golub started playing the Frankie Laine song, “Ghost Riders in the Sky.” Notes filled the halls of the Rehabilitation Hospital of the Northwest in Post Falls. They were the sweet sounds of recovery.
“At first, I couldn’t move my left hand at all,” Golub said. “It sounded bad, but I never imagined being able to play again.”
The unusual approach of blending music with physical rehabilitation played a critical role in Golub’s recovery, said Dr. Neilly Buckalew, who assisted with Golub’s recovery.
“Musicians’ brains are wired differently,” she said. “The second
I found out he was a musician, I knew this would help him recover from the stroke and it did.”
Buckalew is a physiatrist, a medical doctor who treats a wide variety of medical conditions affecting the brain, spinal cord, nerves, bones, joints, ligaments, muscles, and tendons, using an integrated approach to medicine. Her approach to pain management is different than most.
“I believe strongly in not prescribing narcotic pain medicine,” she said. “We have a real problem in this country with opiate addiction. The sooner we can move away from those prescriptions in a recovery, the better.”
Buckalew also ordered an aggressive regimen of physical therapy —- something Golub embraced with gusto.
“If they said two hours, I would do an extra four,” he said. “Every day I pushed myself.”
The 63-year-old has worn many hats over the years, including real estate broker, substitute teacher, graphic designer and musician.
Last year, Golub created a tribute poster to fallen Coeur d’Alene police officer Greg Moore. His artwork is featured with this sponsored content story.
In addition to his professional and personal accomplishments, Golub almost became a statistic. The Centers for Disease Control says that 795,000 people in the United States have a stroke every year and it estimates 130,000 die of strokes annually.
Alan Golub and his wife went to Northern Quest Resort & Casino on Jan. 23 and nearly cashed in all of his chips. Golub was going for a walk when he began to feel ill. He didn’t get far, collapsing in the hotel. Jim Shaeffer, one of the emergency medical technicians on staff rushed to his side. Golub’s blood pressure was sky high — 256 over 180 — and the EMTs believed he was having a stroke.
“I didn’t feel right and I knew that I was in trouble,” he said. “Luckily, they had EMTs on duty and they were able to get me to the hospital quickly. Ten minutes more and I would have lost my ability to speak; another 10 minutes and I might not be breathing today.”
Golub was treated at Sacred Heart Medical Center in Spokane and the preliminary diagnosis of a stroke was confirmed. He was paralyzed on the left side of his body and he had trouble speaking. Golub was admitted to the Rehabilitation Hospital in order to recover from the stroke.
“Alan is amazing,” Buckalew said of Golub’s recovery. “He’s 120 percent better than when I first saw him. He worked hard and he had a great attitude.”
Today, it would be hard to know Golub had suffered a stroke two months ago. He still walks with the assistance of a walker, but his speech and movement are normal. He is able to crack jokes and he appreciates life.
“I feel like I am totally healed,” Golub said. “I feel stronger every day. I am so grateful for what I have. The people at the hospital were incredible. I am a miracle.”
—
By MARC STEWART – Coeur d’Alene Press
About Ernest Health
Rehabilitation Hospital of the Northwest is part of Ernest Health, a network of rehabilitation and long-term acute care hospitals. Ernest Health hospitals see patients who are often recovering from disabilities caused by injuries or illnesses, or from chronic or complex medical conditions.Read More
Quick Reference Links
• Contact Us• Career Opportunities at this Hospital
• Price Transparency
• About Ernest Health